Local health departments working to protect the nation from COVID-19
As COVID-19 spreads across the United States, local public health departments find themselves on the front lines trying to protect communities from this latest version of the coronavirus, George Roberts Jr. told a National Press Club audience Friday.
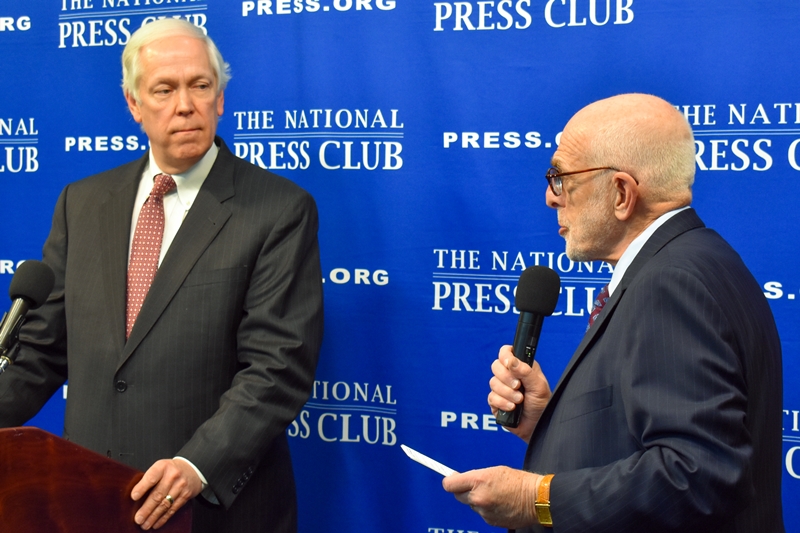
The National Association of County and City Health Officials has nearly 3,000 affiliates, and Roberts, its president, describes them as “the boots on the ground” in the fight against SARS-CoV-2, as the virus is named, and COVID-19, the shortened title of the disease it causes.
After NPC President Michael Freedman introduced him, Roberts praised the nation’s local media for keeping the public current on the respiratory virus that is spread through large droplets from coughing and sneezing. Roberts is also the Chief Executive Officer of the Northeast Texas Public Health District and has more than 35 years of health care experience, mostly in hospital administration.
Roberts reviewed tips for keeping people safe: Repeated hand-washing for at least 20 seconds; not touching your eyes, nose or mouth with your hands; staying home when sick; avoiding contact with people who are sick; not shaking hands; covering your nose and mouth when coughing or sneezing, preferably with a disposable tissue; and regularly cleaning surfaces to avoid virus droplets. He’s heard that this latest virus can last on a given surface from a few hours to nine days.

Reports to date find 80 percent of COVID-19 cases are mild and don’t require hospitalization, while this year’s regular flu season has so far affected up to 45 million Americans, he said. So far, the U.S. has recorded more than 420 COVID-19 cases, according to The New York Times late Saturday night. New York has now declared a state of emergency.
Here are steps local health departments are taking to prepare for an outbreak: Inventorying their preparedness supplies and N95 masks, monitoring, contact-tracing, assessing people at risk (those with heart or lung disease, diabetes) and/or exhibiting symptoms. Finding persons of interest who’ve traveled to/from affected countries or on cruise ships who used ports of entry, and making sure local providers have information they need, and test kits.
Roberts’ affiliates are building relationships with their local police and fire chiefs, emergency management officials, and national partners like the Centers for Disease Control and Prevention so they can coordinate actions in a health crisis. They see their role as “mitigating fear” in their communities. Until now, local health departments viewed themselves as “invisible guardians” of clean water, food safety, and providers of vaccines, but now they find themselves in the spotlight preparing for the unknown.
Seven known coronaviruses exist, according to Roberts, and the first is the common cold. Some other examples: Ebola, SARS in 2002 with more than 8,000 cases and 775 deaths, and MERS in 2012 with 2500 cases and 858 fatalities. Not enough data is available to determine the disease’s mortality rate, no COVID-19 vaccines or anti-virals exist, and no vaccines are expected this year.
